Pigment Dispersion Syndrome and Heterochromia Laser Therapy
Pigment dispersion syndrome (PDS) is an eye condition in which pigment granules are released from the posterior iris surface and circulate inside the anterior chamber. These particles may accumulate on the corneal endothelium, lens, zonules and, most importantly, in the trabecular meshwork. In susceptible patients this process can increase intraocular pressure and lead to pigmentary glaucoma.
In some cases, chronic pigment loss and redistribution also change the way the iris reflects light. As a result, one eye may appear slightly lighter or darker than the other, or sectoral color differences may develop. This form of acquired heterochromia is very different from congenital heterochromia that is present from birth. For a general overview of heterochromia types and causes, you can visit our dedicated page: Heterochromia Treatment.
What Is Pigment Dispersion Syndrome?
In pigment dispersion syndrome, the iris lies relatively close to the lens zonules. Mechanical friction between the iris pigment epithelium and the zonular fibers causes pigment to be released into the aqueous humor. These fine particles are transported by the aqueous flow and may deposit on different anterior segment structures.
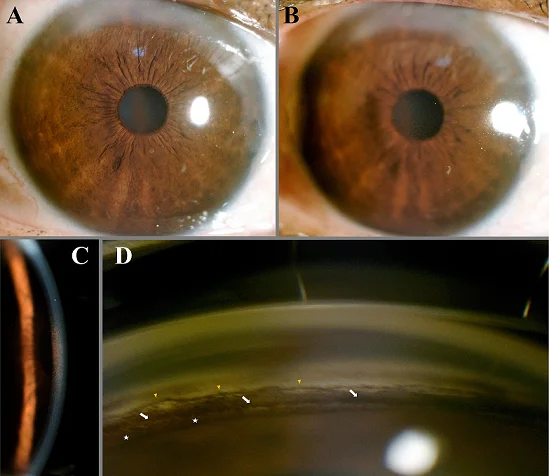
Typical clinical findings include:
- Krukenberg spindle (vertical spindle of pigment on the corneal endothelium)
- Heavy trabecular meshwork pigmentation on gonioscopy
- Pigment deposits on the lens and zonules
- Transillumination defects of the mid-peripheral iris
PDS often affects young myopic patients and may remain asymptomatic for years. The condition becomes clinically important when intraocular pressure increases or when pigment-induced damage to the trabecular meshwork leads to pigmentary glaucoma.
Pigmentary Glaucoma and Ocular Hypertension
When pigment accumulation obstructs the trabecular meshwork, aqueous outflow decreases and intraocular pressure (IOP) may rise. This situation is referred to as pigmentary glaucoma or pigmentary ocular hypertension, depending on whether optic nerve and visual field damage are present.
Patients may report:
- Intermittent blurred vision or halos, especially after exercise
- Eye discomfort or pressure sensation
- Occasional redness or photophobia
However, many patients remain symptom-free until optic nerve damage becomes advanced. For this reason, regular ophthalmologic examinations, optic nerve evaluation and visual field testing are essential once PDS or pigmentary glaucoma is suspected.
How Can Pigment Dispersion Cause Heterochromia?
Chronic pigment release and deposition can subtly change iris appearance. In some eyes, local pigment loss makes a sector of the iris appear lighter. In others, dense pigment accumulation or chronic inflammation may darken certain regions. Over time, this may result in noticeable color asymmetry between the two eyes or within different sectors of the same iris.
Key points that distinguish this from congenital heterochromia are:
- Later onset, usually in young or middle-aged adults
- History of myopia, pigment dispersion or glaucoma treatment
- Associated findings such as Krukenberg spindle and heavily pigmented angles
This type of heterochromia is therefore a sign of an underlying dynamic process rather than a stable, harmless variation from birth.
Diagnosis and Clinical Evaluation
When a patient presents with heterochromia and there is suspicion of pigment dispersion, a complete ophthalmologic examination is required. This typically includes:
- Slit-lamp biomicroscopy to detect pigment deposits and iris transillumination defects
- Intraocular pressure measurement and diurnal IOP profile when indicated
- Gonioscopy to evaluate angle pigmentation and configuration
- Optic nerve head examination and retinal nerve fiber layer imaging
- Standard automated perimetry (visual field testing) in cases with elevated IOP
The aim is to distinguish between benign pigment dispersion without damage and pigmentary glaucoma that already threatens the optic nerve.
Conventional Treatment Options
Management of pigment dispersion syndrome and pigmentary glaucoma must always be individualized. In general, standard glaucoma principles apply:
- Medical therapy: topical pressure-lowering eye drops to reduce aqueous production or increase outflow.
- Lifestyle and activity advice: in selected cases, avoiding extreme exertion that triggers pigment release may be helpful.
- Laser or surgical procedures: when medical therapy is insufficient, different techniques (such as laser trabeculoplasty or filtering surgery) may be considered to improve outflow and protect the optic nerve.
These therapies aim primarily to control intraocular pressure. They are not designed to correct iris color differences, although stabilization of pigment release can sometimes prevent further asymmetry.
Laser Therapy in Pigment Dispersion Syndrome at My Lumineyes
In our clinic, we have developed a selective laser approach for carefully chosen patients with pigment dispersion or pigmentary glaucoma accompanied by noticeable heterochromia. The goal of this therapy is twofold:
- to optimize pigment removal and improve aqueous outflow dynamics, and
- to achieve a more balanced and natural iris appearance when asymmetry is caused by pigment overload or sectoral loss.
This laser protocol is not a standard glaucoma procedure and is not intended to replace established treatments when they are indicated. Instead, it is used as an adjunctive, individualized therapy after full diagnostic work-up and discussion of risks and benefits with the patient.
Our experience suggests that, in selected cases, laser modulation of iris pigment may both support pressure control and reduce the visual contrast of heterochromia. However, the response is patient-specific, and complete color equalization cannot be guaranteed. Protecting the optic nerve and maintaining visual function always comes before cosmetic goals.
Who May Be a Candidate for This Laser Therapy?
Potential candidates are patients who meet all of the following criteria:
- Documented pigment dispersion syndrome or pigmentary glaucoma
- Visible heterochromia or marked iris color asymmetry related to pigment changes
- Comprehensive examination excluding other causes of iris color change (inflammation, tumors, drug-induced effects, etc.)
- Realistic expectations regarding both glaucoma control and cosmetic outcome
Every case is evaluated individually. In some patients, conventional glaucoma management alone remains the safest and most appropriate option.
Limitations, Risks and Follow-Up
As with all laser procedures in the anterior segment, there are potential risks, including transient inflammation, pressure spikes, or, rarely, structural changes. For this reason, treatment is performed under strict indications and with close follow-up. Patients are monitored for:
- Intraocular pressure changes immediately after the procedure
- Inflammatory response and anterior chamber reaction
- Optic nerve status and visual field over time
- Stability of iris color and symmetry
This page is provided for informational purposes only and does not replace a personal consultation. Any decision about laser treatment for pigment dispersion or heterochromia must be made together with an experienced ophthalmologist who has access to your full medical history.
FAQ: Pigment Dispersion Syndrome
Is pigment dispersion syndrome always dangerous?
Not always. Some patients remain stable for years, but pigmentary glaucoma may develop silently. Regular examinations are essential.
Can pigment dispersion cause heterochromia?
Yes. Chronic pigment release or sectoral pigment loss may change iris appearance and create color asymmetry.
Does selective laser therapy fix heterochromia?
It may soften color asymmetry in selected cases, but complete equalization is not guaranteed. Protecting the optic nerve remains the priority.
When should a patient seek urgent care?
Sudden eye pain, rapid vision decline, halos, nausea, or marked redness require immediate ophthalmologic evaluation.
Can pigment dispersion–related heterochromia return to normal?
In some mild cases, color differences may become less noticeable over time as pigment release stabilizes. In others, asymmetry persists. Any sudden change in iris color or new visual symptoms should always be evaluated by an eye specialist.
Does laser therapy replace glaucoma drops or surgery?
No. Laser procedures are usually considered in addition to, not instead of, standard glaucoma treatments. Many patients still require pressure-lowering eye drops or, in advanced cases, surgical intervention.






